| Characteristic | Detail |
|---|---|
| Active Ingredient | Apixaban |
| Usage | Prevention of stroke and systemic embolism in patients with nonvalvular atrial fibrillation; Treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE); Prevention of recurrent DVT and PE |
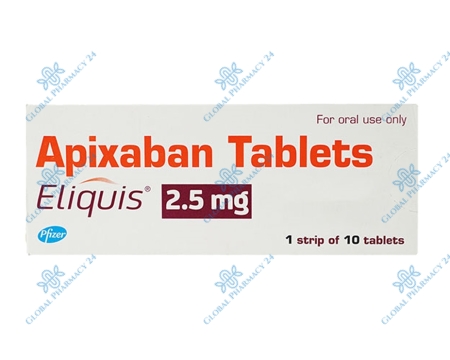
| Dosage Form | Oral tablets (2.5 mg, 5 mg) |
| Duration of Effect | 12-24 hours |
| Side Effects | Bleeding, nausea, anemia, rash, allergic reactions |
Understanding Eliquis
Eliquis, known generically as Apixaban, is a revolutionary anticoagulant medication that plays a crucial role in preventing blood clots in patients with nonvalvular atrial fibrillation. Its significance extends beyond just atrial fibrillation patients; it is also used in the treatment and prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE), conditions that pose serious risks to individuals' health worldwide. By inhibiting specific proteins involved in the blood coagulation process, Eliquis efficiently reduces the risk of stroke and blood clot formation without the need for routine blood monitoring, marking a significant advancement over traditional therapies.
The advent of Eliquis has been a milestone in cardiovascular medicine, offering patients an effective and safer alternative to older anticoagulants like warfarin. Unlike warfarin, which requires frequent dose adjustments and monitoring, Eliquis provides a fixed-dose regimen that simplifies treatment protocols and enhances patient compliance. This ease of use, combined with its effective risk reduction capabilities, underscores the importance of Eliquis in modern medicine, particularly in the management of diseases associated with thromboembolic events.
What is Eliquis?
Eliquis is an oral anticoagulant that belongs to the class of drugs known as Factor Xa inhibitors. It is specifically designed to prevent the formation of harmful blood clots in the arteries and veins, which can lead to stroke or embolism. By selectively inhibiting Factor Xa, a critical enzyme in the clotting process, Eliquis effectively reduces the risk of clot-related complications in patients with certain cardiovascular conditions without the need for the dietary restrictions and constant monitoring associated with older anticoagulants.
How does Eliquis work?
Eliquis operates by directly inhibiting Factor Xa, an enzyme vital to the clotting cascade that leads to the formation of thrombin and eventually fibrin, the main components of blood clots. This mechanism of action disrupts the clotting process at a crucial stage, preventing the formation of clots while maintaining sufficient coagulation to reduce the risk of bleeding complications. This targeted approach provides a balance between preventing clot formation and minimizing bleeding risks, setting Eliquis apart from other anticoagulants.
Importance of Eliquis in Modern Medicine
The introduction of Eliquis has significantly impacted the management of thromboembolic disorders, providing a safer and more convenient treatment option for patients. Its effectiveness in reducing the risk of stroke and systemic embolism in individuals with nonvalvular atrial fibrillation, along with its use in the treatment and prevention of DVT and PE, has established Eliquis as a cornerstone in the prevention of clot-related diseases. The drug's favorable safety profile, coupled with its ease of use, supports its growing importance in contemporary medical practice.
Detailed Composition and Properties of Eliquis
Eliquis is composed of Apixaban as its active ingredient, a potent Factor Xa inhibitor that offers a novel approach to anticoagulation therapy. This composition is designed to provide consistent and predictable anticoagulation, reducing the risk of stroke and systemic embolism in patients with atrial fibrillation not caused by heart valve disease. Apixaban's pharmacokinetic properties, including its oral bioavailability, half-life, and renal and hepatic metabolism, contribute to its effectiveness and safety profile, making it a preferred option for long-term anticoagulation therapy.
Examining the properties of Eliquis reveals its distinct advantages over traditional anticoagulants. Its rapid onset of action and predictable pharmacodynamics allow for a fixed dosing regimen without the need for INR monitoring, a significant improvement in the management of patients requiring anticoagulation. Additionally, Eliquis exhibits a lower risk of major bleeding, including intracranial hemorrhage, compared to other anticoagulants, further solidifying its role in modern therapeutic strategies for preventing thromboembolic events.
Breaking down the components of Eliquis
The primary component of Eliquis, Apixaban, is complemented by several inactive ingredients that ensure the drug's stability, bioavailability, and ease of administration. These include lactose, microcrystalline cellulose, sodium lauryl sulfate, and magnesium stearate, among others. This composition not only facilitates the drug's absorption and effectiveness but also ensures that Eliquis can be administered in a patient-friendly tablet form, available in two dosages to accommodate varying patient needs and treatment protocols.
Examining the properties of Eliquis
Eliquis distinguishes itself with a well-balanced profile of absorption, distribution, metabolism, and excretion. Its oral bioavailability is approximately 50%, with peak plasma concentrations occurring 3 to 4 hours post-dose. Eliquis is predominantly metabolized in the liver, involving CYP3A4-mediated pathways, and is excreted through both renal and fecal routes. This pharmacokinetic profile supports the drug's twice-daily dosing regimen, providing effective and sustained anticoagulation throughout the day and night.
Recognized Side Effects
The recognized side effects of Eliquis encompass bleeding complications, including minor bleeding like nosebleeds and bruising, as well as more serious bleeding events such as gastrointestinal bleeding or intracranial hemorrhage. Non-bleeding side effects are less common but can include nausea, anemia, rash, and allergic reactions. Patients and healthcare providers should be vigilant for any signs of bleeding and other adverse reactions, especially in individuals with increased risk factors for bleeding.
Severity and likelihood of each side effect
While the majority of patients taking Eliquis do not experience severe side effects, the likelihood and severity of bleeding complications can vary based on several factors, including the patient's age, renal function, and concomitant use of other medications that affect hemostasis. Minor side effects like nausea and anemia are generally manageable and often resolve with continued treatment or minor adjustments to therapy.
Comparing the effects of Eliquis with other similar drugs
When compared to traditional anticoagulants like warfarin, Eliquis demonstrates a lower risk of major bleeding, particularly intracranial hemorrhage. Additionally, unlike warfarin, Eliquis does not require regular blood monitoring or dietary restrictions, offering a significant advantage in terms of patient convenience and quality of life. However, in situations requiring rapid reversal of anticoagulation, the availability of specific reversal agents for warfarin can be a benefit not yet fully matched for Eliquis, although specific reversal agents for Eliquis are under development and have begun to be introduced.
Precautionary Measures When Using Eliquis
Ensuring the safe use of Eliquis involves taking specific precautionary measures, particularly regarding its interaction with other medications and its use in patients with certain pre-existing conditions. Healthcare providers must thoroughly review a patient's medication history to avoid potential interactions that could increase the risk of bleeding. Similarly, careful consideration should be given to patients with renal or hepatic impairment, as these conditions can affect the metabolism and excretion of Eliquis, necessitating dose adjustments or alternative treatments.
Patients with a history of bleeding disorders, undergoing surgery, or pregnant and nursing women require special attention when considering Eliquis therapy. In these cases, the benefits of reducing the risk of thromboembolic events must be carefully weighed against the potential risks of bleeding. Education on recognizing signs of bleeding and understanding when to seek medical attention is crucial for all patients taking Eliquis.
Interaction of Eliquis with other medications
Eliquis can interact with other medications, particularly those that affect coagulation, such as nonsteroidal anti-inflammatory drugs (NSAIDs), antiplatelet agents, and other anticoagulants, increasing the risk of bleeding. Additionally, drugs that affect the cytochrome P450 3A4 enzyme and P-glycoprotein transporter can alter the levels of Eliquis in the body, potentially leading to increased exposure and risk of bleeding or decreased efficacy. Patients and healthcare providers must manage these interactions through careful medication selection and monitoring.
Special precautions for patients with certain conditions
Patients with renal or hepatic impairment require special consideration when using Eliquis, as these conditions can significantly impact the drug's pharmacokinetics. In patients with moderate to severe renal impairment or significant hepatic dysfunction, dose adjustments may be necessary, or alternative anticoagulant therapies may be more appropriate. It is essential to evaluate each patient's renal and hepatic function before initiating Eliquis therapy and periodically thereafter.
Advice for Patients with Renal Impairment
For patients with renal impairment, careful monitoring and potential dose adjustment of Eliquis are necessary. The drug's clearance is partially dependent on renal excretion; therefore, impaired renal function can lead to increased plasma concentrations of the drug, elevating the risk of bleeding. Dosing recommendations for patients with varying degrees of renal impairment are provided in the prescribing information to ensure safe use.
Advice for Patients with Hepatic Impairment
Eliquis is not recommended for patients with severe hepatic impairment due to the risk of bleeding and the lack of clinical study data in this population. For patients with mild to moderate hepatic impairment, no dose adjustment is typically required, but these patients should be closely monitored for signs of bleeding. The decision to use Eliquis in patients with hepatic impairment should be based on a thorough assessment of the benefits and risks.
Safety of Eliquis for Pregnant and Nursing Women
The safety of Eliquis during pregnancy and lactation has not been established. Eliquis should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. For nursing women, caution is advised, and a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
Usage among Children and Elderly
The safety and efficacy of Eliquis in pediatric patients have not been established. In elderly patients, careful dose adjustment and monitoring are essential due to the increased risk of bleeding and potential renal impairment in this population. Elderly patients may require lower doses based on renal function assessment.
Understanding the Prescribed Usage of Eliquis
Eliquis is prescribed for the prevention of stroke and systemic embolism in patients with nonvalvular atrial fibrillation, as well as for the treatment and prevention of DVT and PE. Its use is based on a fixed-dose regimen, which simplifies treatment and enhances patient compliance. Understanding the correct dosage and administration of Eliquis is crucial for achieving the desired therapeutic effects while minimizing the risk of adverse effects.
Understanding the Dosage and Administration
The standard dosage for Eliquis varies depending on the indication. For prevention of stroke and systemic embolism in patients with nonvalvular atrial fibrillation, the typical dosage is 5 mg taken twice daily. For patients with at least two of the following characteristics: age ≥80 years, body weight ≤60 kg, or serum creatinine ≥1.5 mg/dL, the recommended dose is reduced to 2.5 mg twice daily. The dosing for the treatment of DVT and PE, and the prevention of recurrent DVT and PE, also follows specific guidelines. Patients should take Eliquis exactly as prescribed by their healthcare provider, and never change their dose or stop taking the medication without consulting their provider.
Dosage-related Precautions
While Eliquis is effective in reducing the risk of stroke and systemic embolism, it is essential to follow dosage-related precautions to prevent potential adverse effects, primarily bleeding. Patients should inform their healthcare providers about all medications they are taking, including over-the-counter drugs, vitamins, and herbal supplements, to avoid interactions that could affect Eliquis efficacy or increase bleeding risk. Additionally, patients should be aware of the signs and symptoms of bleeding and report any such occurrences to their healthcare provider immediately.
Research and Clinical Findings on Eliquis
Extensive research and clinical trials have demonstrated the efficacy and safety of Eliquis in the prevention and treatment of thromboembolic disorders. Eliquis has been compared to other anticoagulants in several large-scale, randomized, controlled trials, showing significant benefits in reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation, with a comparable or lower rate of major bleeding.
Key clinical findings highlight Eliquis's role in improving patient outcomes in the management of atrial fibrillation and venous thromboembolism. The drug's favorable safety profile, including a reduced risk of intracranial hemorrhage and fatal bleeding compared to warfarin, supports its use as a first-line therapy for eligible patients. Ongoing studies continue to investigate the long-term benefits and potential new indications for Eliquis, further solidifying its position in cardiovascular medicine.
Clinical Trial Results
The ARISTOTLE and AVERROES studies are among the pivotal trials that have established the efficacy and safety of Eliquis. In these studies, Eliquis demonstrated a significant reduction in the risk of stroke and systemic embolism in patients with atrial fibrillation compared to warfarin, with fewer bleeding incidents. These results have been instrumental in guiding clinical practice and have led to the widespread adoption of Eliquis as a preferred anticoagulant for many patients.
Summary of Key Clinical Findings
Key clinical findings from research on Eliquis include its superior efficacy in stroke prevention, lower risk of major bleeding, and reduced mortality compared to warfarin. Additionally, Eliquis has shown benefits in the treatment and secondary prevention of DVT and PE, offering a valuable option for patients with these conditions. The consistent outcomes across diverse patient populations and the drug's well-defined safety profile underscore its important role in contemporary anticoagulant therapy.
Understanding the Role of Eliquis in Stroke Prevention
Eliquis plays a critical role in the prevention of stroke, particularly in patients with nonvalvular atrial fibrillation, where it reduces the risk of stroke by preventing clot formation. Its mechanism of action, selectively inhibiting Factor Xa, targets a key step in the coagulation cascade, effectively reducing the potential for thrombus formation without significantly increasing the risk of bleeding. This balance of efficacy and safety is a crucial factor in the management of patients at risk for stroke.
The importance of Eliquis in stroke prevention extends to its ease of use and favorable safety profile compared to traditional anticoagulants. Its fixed-dose regimen eliminates the need for routine INR monitoring, simplifying treatment and improving patient adherence. These attributes, combined with its demonstrated clinical efficacy, make Eliquis an essential tool in the prevention of stroke in patients with atrial fibrillation and other risk factors for thromboembolism.
The Connection between Eliquis and Stroke Prevention
Eliquis's ability to significantly reduce the risk of stroke in patients with nonvalvular atrial fibrillation is a key aspect of its clinical utility. By directly inhibiting Factor Xa, Eliquis decreases the formation of blood clots, which are a primary cause of stroke in this patient population. Its role in stroke prevention is supported by extensive clinical data, highlighting its effectiveness and safety in reducing stroke risk compared to other anticoagulants.
Effectiveness of Eliquis in Stroke Prevention
The effectiveness of Eliquis in stroke prevention has been consistently demonstrated in clinical trials, where it has shown to provide significant protection against stroke and systemic embolism in patients with nonvalvular atrial fibrillation. Its advantages over traditional anticoagulants, such as warfarin, include a lower risk of major bleeding, particularly intracranial hemorrhage, and the absence of the need for dietary restrictions or frequent dose adjustments, making it a superior choice for many patients.
Comparative analysis: Eliquis versus other Stroke Prevention Drugs
In comparative analyses, Eliquis has been shown to offer several advantages over other stroke prevention drugs, including a lower risk of bleeding, particularly intracranial hemorrhage, and greater convenience due to the lack of need for regular blood monitoring. Studies comparing Eliquis with other anticoagulants, such as warfarin, dabigatran, and rivaroxaban, have consistently demonstrated its efficacy and safety, reinforcing its role as a preferred option for stroke prevention in patients with nonvalvular atrial fibrillation.
FAQs Eliquis
What is Eliquis?
Eliquis is a prescription medication used to reduce the risk of stroke and blood clots in people with atrial fibrillation, a type of irregular heartbeat, as well as for the treatment and prevention of deep vein thrombosis and pulmonary embolism.
How does Eliquis work?
Eliquis works by inhibiting the activity of certain clotting proteins in the blood, thereby preventing the formation of blood clots. This helps reduce the risk of stroke and other clot-related conditions.
Who can take Eliquis?
Eliquis is typically prescribed to adults who have atrial fibrillation, deep vein thrombosis, or pulmonary embolism. However, its use should be determined by a healthcare professional based on individual medical history and risk factors.
What are the possible side effects of Eliquis?
Common side effects of Eliquis may include bruising, bleeding, and nausea. Serious side effects may include severe bleeding or allergic reactions. It's important to consult a healthcare provider if any concerning side effects occur.
How should Eliquis be taken?
Eliquis should be taken exactly as prescribed by a healthcare provider. It is typically taken orally, with or without food, as directed. It's important not to exceed the prescribed dosage and to follow all instructions provided by the prescribing physician.
Can Eliquis interact with other medications?
Yes, Eliquis can interact with other medications, including certain blood thinners, antifungal drugs, and antibiotics. It's important to inform healthcare providers about all medications, supplements, and herbal products being taken to avoid potential interactions.
What should I do if I miss a dose of Eliquis?
If a dose of Eliquis is missed, it should be taken as soon as possible unless it is close to the time for the next scheduled dose. In such cases, the missed dose should be skipped, and the regular dosing schedule should be resumed. Double doses should not be taken to make up for a missed dose.